The How and Why: Increasing the Adoption of Agile Processes in Healthcare?
Healthcare has followed a top-down approach for many years. This incorporates a waterfall methodology- a vertical hierarchical structure that can result in decreed orders rather than questions being asked. The latter tends to empower workers. However, the former can cause a loss of autonomy, which has been demonstrated as a critical problem in medical staff burnout and disengagement.
In some cases, a workplace where workers are seen not as "co-participants" but as "resources" is detrimental to staff development. In a top-down waterfall approach, groups are often separated or siloed, lowering collaboration where processes are not integrated. Staff can become demoralised by this isolation in effect and do not function well when seen as "just worker bees".
The World Health Organisation (WHO) in 2019 recognised the adverse occupational contribution of some workplace cultural practices when burnout was accepted as a syndrome of the workplace. Conversely, Agile practices plan for and embrace change. They are adaptive and proactive. This can give teams the flexibility to adapt to changing needs or situations.
Also, an Agile-infused workplace can give greater flexibility to incorporate new knowledge, new tools and new technology. Agile practices have been very much required this year in global healthcare to respond quickly to the pandemic. Change has been amazingly adopted, and all healthcare planners and facilitators should be congratulated for leading us in all these areas.
This response is perhaps an example of the collaborative redesigned healthcare workforce of the future. This is also where data informatics helps lead behavioural health changes to enhance significantly patient and staff engagement. Another analogous model is the PDSA: Plan-Do-Study-Act. This improvement model also achieves definable goals and readily visible deliverables. These changes in work practices must be shared with all workers to increase collaboration and buy-in. To have these practices or methodologies used only by administrative/executive staff is no longer good enough.
So, how can the Agile process be applied across healthcare platforms to all medical and allied medical staff workforces? Firstly, any healthcare organisation's senior leaders / medical influencers must lead the way. They must be very familiar with the process and should openly support this form of work practice. They should be able to help set up inclusive teams that can adopt different Agile strategy techniques, which are tested for efficiency, deliverability and functionality. Finally, sharing must be transparent and equitable.
The focus is on obtaining products or services that are in demand, innovative, and required to improve conditions and outcomes for the patient or the Healthcare team. It is worth restating; clinical medical staff must be involved in these Agile processes. That includes Nurses and allied health professionals.
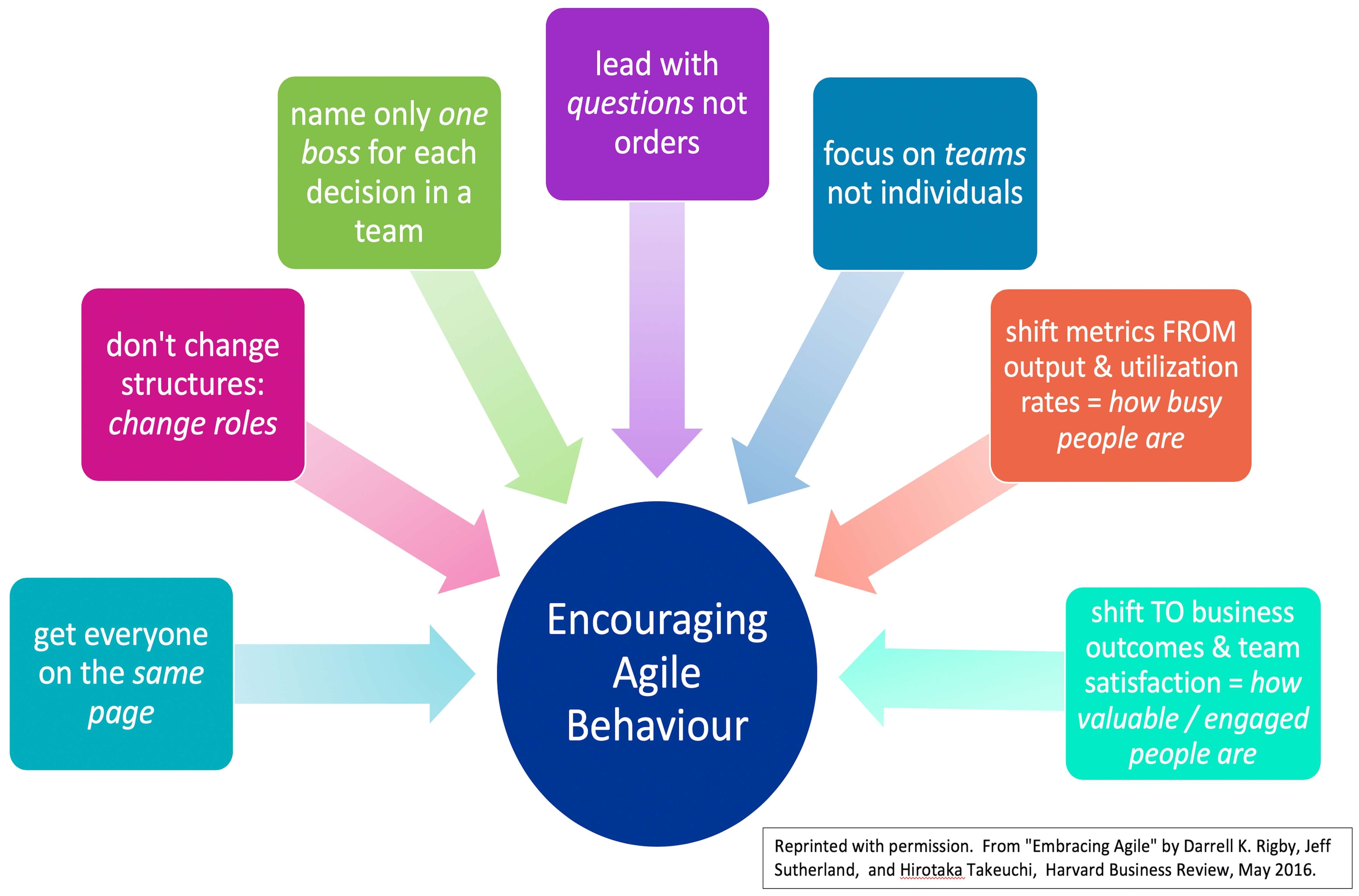
The reason to encourage Agile practices in the medical, nursing and allied health professions is to increase staff involvement, particularly in small groups. That is where natural creativity occurs. The groups should have 6-8 people. They need to work on projects that matter, to be more responsible for fundamental changes in the organisation.
Being involved in creative processes promotes real benefits for staff and, thus, tangible patient benefits. This improves staff buy-in and creates strong cross-platform functional teams. This is very beneficial for the organisation as a whole, increasing corporate reputation and demonstrating the forward-thinking nature of the executive team. This will be a win-win for all…
It is increasingly apparent that general medical staff are not included in these decision-making and problem-solving projects, as they have been deemed "need to care for their patients." Sure, specific medical staff mem has been involvedbers have been involved, but they have tended to be co-opted to echo a particular type of administrative narrative.
What is needed is a democratic universal approach. Programs that are available to all medical, nursing and allied medical staff. People who want to opt-in. Not programs where staff apply then, only a small number are selected. That breeds elitism.
The plight of medical graduates exemplifies where significant changes could and should occur. The younger medical graduates should be given leadership and development programs, life coaching, agile coaching and mentorship. We will be discussing all of these issues shortly.
This is to counteract the burden that often starts in the intern year of a medical graduate. After long years of studying medicine, the graduates are "rewarded" by becoming glorified clerical staff. This leads to an overwhelming tide of excessive demands for administrative paperwork, electronic medical record keeping and a required over-commitment to work hours. No wonder medical burnout levels have run at 40-50% in extensive demographic and occupational studies worldwide in the last ten years.
In summary, we at Creative Thinking Institute believe a hybrid model of the incumbent traditional waterfall methodology must be paired with specific Agile methodology projects. Where the gains are freely shared, people are valued for their contributions; staff are enthused in teams and empowered to express their opinions and ideas.
Before the administrators defend their current position, let me say- you are doing and have done a great job. The gains in medicine in the last 20 years can partly be due to the careful application of corporate principles and metrics.
However, the cost has indeed been borne by many of the staff. Those that have been suffering in silence, those that have been acting out, and those that have been burning out, we must accept that the time is now to change to evolve into a better system. So let's collaborate to look at how we can retune the system. Can we utilise Agile practices as a tool to aid the necessary repairs?
This is critical because adopting these components of Agile practice (initially on a smaller controlled scale) may not only improve staff retention but also heighten staff morale, improve patient outcomes and build a resilient, adaptive cross-cultural meshwork fabric through reducing staff burnout levels.
This is how we should specifically combat the loss of autonomy, disillusionment, emotional exhaustion and career stalling, which is so prevalent in the medical and allied medical professions.
This is how we can create a renewed workforce in the future.
Further discussion blog: Pitfalls and Problems Leading to Failures of Agile Processes in Healthcare