Re-engineering the medical and corporate mindset
Advancements in all facets of healthcare have delivered great strides over the last twenty years. This progress is currently being led, in part, by significant technological innovations. This is well demonstrated in the computer-driven pattern recognition of medical imaging and pathological tissue specimens. Add to this the increasingly sophisticated understanding of molecular and nano-biology, and you can readily appreciate our new era.
Next are the contributions of increased genomic sequencing, the widespread uptake of operative robotics, and real-time surgical image-guided data acquisition. One can visualise all these contributing to a comprehensive, precise point of care (POC) service.
However, despite these welcome changes, we are now, in 2020, at a potential central inflection point. The medical model is being re-fashioned with a decentralised twist. Care will gradually move away from the outpatient clinics of large significant hospitals or the rooms of private practitioners to an individual’s home.
The increasing use of the Internet of medical things (IoMT) combined with 5G+ telecommunications will push this next phase to where patients can genuinely access medical care on their terms. This disruptive model will allow patients to obtain consultations at their chosen time. With the increasing use of telemedicine, pushed quickly further by the advent of Covid-19, patients will be and have already become more enabled to see a medical practitioner at any time of the day or night. Thus, the triad becomes, who they want, how they want and when they want.
Anytime consultations may be provided in the not-too-distant future entirely by computer-augmented physicians in another part of the world. Similar changes will be effected for simple diagnostic procedures. A home otoscope, ultrasonic stethoscope or handheld ophthalmoscope will stream images to available pattern recognition databases to provide immediate diagnostic results and treatment recommendations.
Add disruptive techniques such as image-guided light analysis of capillary blood slides for complete blood counts (SightDX corporation, Israel), making the process more technologically accurate. These are all happening in many countries across the world today. The role of the medical practitioner will continue to evolve. Still, the profession needs to pre-empt these technological changes to provide the most relevant impact and positive future contributions.
Indeed, in this worldwide setting, medical practitioners have been demonstrated as having high levels of disengagement, emotional exhaustion and loss of purpose over the last ten years. The professions will require re-engineering their medical or corporate mindset* to fully function in this era of significant change. As these changes have occurred, the autonomy of the medical profession, for example, has been gradually decreasing.
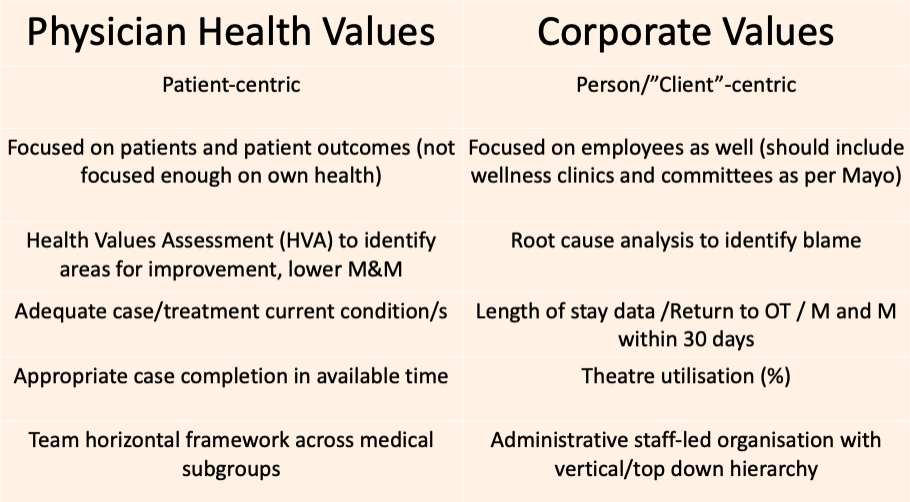
Medical administrations have, by necessity, become more complex and multi-layered. The increasing divide between patient-centric medical models and the required corporate-centric administrative models figured below, has become more readily apparent. Whilst both components are essential in the modern medical workforce, there is a real need for all stakeholders to identify that.
Indeed, we are both on one coin, just on different sides. It requires us to metaphorically turn over the cash to assess the perspective of those around or “opposite” us. Importantly, this need for collaboration will ultimately provide the most significant aid in developing a renewed medical or corporate mindset.
There may be an observable, increasingly disruptive behaviour pattern for physicians that have demonstrated increasing levels of disengagement and despair. The development of abnormally high-stress levels can adversely affect a physician’s performance levels. This, as research repeatedly shows, can increase the frequency of medical errors and adverse medical outcomes.The expressed central aim of Creative Thinking Institute: CTI is to decrease abnormally high-stress levels in the medical/corporate professionals, to improve patient/client outcomes specifically.
One of the pushes over the last ten years has been an attempt to decrease medical error rates by identifying and subsequently re-directing aberrant behaviour patterns in medical and nursing staff. Whilst in itself an initial logical conclusion, with the execution consisting of the development of professional accountability programs, the results have arguably been disappointing. These measures may overlook the reality that disruptive practitioners frequently, in themselves, act out and, when assessed objectively, need our attentive care.
Disruptive behaviour can be a valuable marker that the individual is not coping with and is developing increasing decompensation, emotional exhaustion and depersonalisation. Having stated the above, there is no doubt that the overall corporate and medical culture has seen a dramatic decrease in harassment and bullying in the workplace over the last ten years. All administrations and workers are to be thanked and applauded for their efforts to combat this pervasive issue. Society has changed dramatically in our ability and willingness to call out behaviour that is entirely unacceptable and demeaning to any human being.
The degree of individual decompensation can be objectively measured on scales like the Maslach burnout inventory, Perceived Stress scale and Visual Analog scales of career satisfaction. Multiple studies have identified the reliable, validated use of different measures to quantify increased workplace stress levels, leading to some degree of medical or corporate burnout. These and other scores have been applied to the medical profession to give relatively consistently high overall levels of decompensation to some degree(40-45%USA).
In addition, scores on the stigma of medical burnout demonstrate there is a real stumbling block to open discussion and dialogue in this domain. Understandably, people who are not coping will go to great lengths to conceal this. There is an ever-present fear of reputational damage, loss of referrals, increasing chance of litigation and loss of employment. There is no greater need in the medical or corporate professions than to eliminate this stigma for discussing or expressing personal burnout. We are all human and must show each other tolerance, empathy, compassion and support. This has unfortunately been slow to surface, as the level of comfort to deal with this openly has been low- as in all areas of society. At CTI, we believe this will dramatically change over the current decade as mental health emerges as a right for all to be protected and enhanced.
More simple stop-gap measures to help colleagues have been expounded as beneficial, with various calls to “simply adjust”, to “develop greater resilience”, or practice more comprehensive coping skills, including meditation, yoga and mindfulness. These practices are indeed essential in their own right and should naturally be a part of any well-balanced lifestyle. However, increasing one’s resilience alone has been advocated so frequently that the medical profession has increasingly recoiled from what is loosely called the “R” word. The focus on stability has understandably created impressions that the physician is in some way weak or incompetent. This is far from the truth and underlies societal problems with accepting the need to realistically and openly discuss our mental health status. In this decade ahead, significant advances in medical and corporate well-being could be made if we can embrace the understanding that personal mental health is central and vital to us all. Caregivers need to be fully functional, well-grounded and able to adopt techniques that are shown to improve their mental well-being. No different to the need in our general health to maintain normal blood pressure, good fasting blood sugar or low LDL cholesterol levels.
To create real, lasting change, it is now very appropriate to take a step back and re-analyse the big picture. Professional accountability programs have looked to address those practitioners causing disruption but do not attempt to create purpose-driven educative gains. The time is now to re-address these imbalances. By objectively assessing and measuring burnout in large cohorts of the medical and corporate demographic, the provision of specific interventions can be thoroughly studied to determine the most valuable measures. This is the particular field of interest of the Creative Thinking Institute.
Increasingly over the last five years, studies have assessed Emotional Intelligence – EQ levels in medical students, medical residents, corporate employees and physicians. Findings reveal (understandably) higher levels of EQ in females, with varying levels in different training or career progression time frames. The correlation of higher EQ with improved physician-patient or corporate-client communication can lead to higher patient/client satisfaction and lowered physician / corporate employee stress levels. This has already been readily demonstrated.
The individual components of EQ are variously described but most commonly, as outlined by Daniel Goleman, include improved self-awareness, self-regulation, motivation, empathy and social and interpersonal skills.
In the rapid change of this technological age, it appears, and is also our proposal at Creative Thinking Institute, that another metric is becoming more critical. That is the Adaptability Quotient: AQ, and we will look more deeply into this in another blog post.